Why People with Eating Disorders Need Our Compassion
 Why do some people develop an eating disorder like anorexia, bulimia, or compulsive overeating or binging?
Why do some people develop an eating disorder like anorexia, bulimia, or compulsive overeating or binging?
When we see someone refusing to eat or eating into obesity, the temptation is to criticize or correct them.
“Just stop it! Can’t you see you’re hurting yourself?”
But criticism is the last thing a person with an eating disorder needs.
If we want to help those suffering to recover, understanding and compassion are powerful tools. That is why we all need to learn about the nature of eating disorders. Then, more of us can offer health-building compassion.
Why Do Eating Disorders Develop?
Eating disorders, like drug or alcohol use and self-harming behaviors—are very often about self-regulation of emotion. Men and women of all ages can and do develop them.
People use, abuse, or restrict food, or turn to opiate addiction, substance abuse or self-harming behavior to cope with intolerable or overwhelming feelings and thoughts.
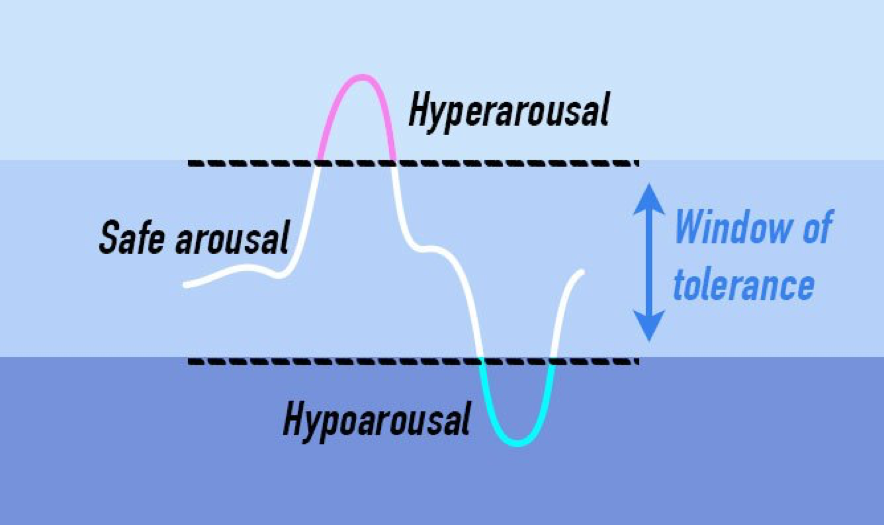
Imagine of three zones of emotional energy. The middle zone represents a window where emotions and thoughts feel tolerable and make sense to us, where we can think and feel at the same time. Our reactions can adapt to a situation. This is the window of tolerance of emotions.
The top zone represents a heightened state of almost pure feeling, including panic, impulsivity, racing thoughts, anger, and a feeling of lack of safety – all of which feels overwhelming. Therapists call this hyperarousal.
The bottom zone is a flat, dull, numb state called hypoarousal. It includes times of no energy, the inability to think, feelings of disconnection and being shut down and can include shame and the inability to say no.
When emotions rise or fall outside the window of tolerance, it is extremely hard to live and behave in healthy ways. Outside the safe zone, people struggle to maintain a sense of well-being. When emotions are too intense, or too suppressed, a person needs a way to bring them back into a level they can live with. This is especially true for trauma survivors. Their nervous systems have learned to be constantly prepared for danger. This response to past hurts and pains is deeply embedded.
The Link Between Eating Disorders and Childhood Trauma
Trauma — especially when it occurs in childhood — dramatically increases the risk that a person will struggle with chronic hypoarousal or hyperarousal throughout life. Studies show that the more types of traumatic experiences in childhood, the higher the risk that addiction, eating disorder, or self-harming behavior will occur.
In fact, the origin of the landmark Adverse Childhood Experiences (ACE) Study began in an obesity clinic. Dr. Vincent Fellatti noticed that more than half of his patients were dropping out of his weight loss program even though they were losing weight well. He wanted to know why, so he interviewed some of those who left.
What he found was a high incidence of sexual abuse among obese patients, which often occurred when they were children. After the abuse, their weight skyrocketed and remained high.
Some people with disordered eating behaviors are likely to have a history of trauma (physical, sexual, or attachment trauma) and are trying to use body size for protection in some way (for example, restricting to be more invisible or binging to be overweight and less attractive to abusers). Others use food as a mechanism of self-soothing or something they have control over.
The use of addictive behaviors (food, drugs, alcohol, gambling, sex, etc.) comes from the desperation of those suffering with trauma symptoms to find a solution for chronic emotional distress. People use substances or harmful behaviors to help them not feel as bad, because otherwise, they feel either intolerably reactive or numb.
Gaining a Sense of Control
How do self-harming, addiction, or eating disordered behaviors help people cope with too much or too little reactivity in their inner world?
No matter what eating disorder or what self-regulation mechanism people use, people turn to them to get some sort of feeling of control over their lives. It’s like when a person sees a wave of emotion crashing – they don’t know what to do. You’re feeling so out of control, or something feels so overwhelming or panic inducing, you turn to something else you can control. “Well, I can control what I put in my mouth.”
Restricting or binging with food for some people brings them down from hyperarousal. For others, it brings them up from a low.
The Longing to Stop Feeling So Bad
The issue around those who use food is not just about appearance or even about appearance at all. I believe that anorexia or bulimia isn’t as much about looking like the model in the magazine as it is about wanting to feel like her (or how we imagine she feels). Restricting food becomes a mechanism for feeling better, not because it makes a person feel beautiful, but because having at least some measure of control helps that person to not feel as bad.
It’s a self-soothing mechanism. One result of using food restriction or binging and purging, is that to be able to do it, you must disconnect your awareness from your body. Whether you’re starving yourself or overeating, to succeed, you are not able to check in and hear the health-promoting signals from your body.
The brain-body disconnect can give some measure of relief from the physical symptoms of anxiety or shame. But the problem then becomes dissociation from healthy signals, too.
The Role of Re-Framing in Treating and Healing from Eating Disorders
Treatment for eating disorders is not about food. It’s not about focusing on a diet or monitoring what people eat. It’s about what the eating behavior means to the person.
Sometimes, the client and therapist learn that food restriction is about a wish to become invisible. Sometimes eating very little means a person wants to be small. To cope with a history of trauma, they just don’t want to be noticed.
In therapy, we talk about why that behavior makes sense. When we re-frame the behavior by asking why it’s there, we can empathize. It is not ‘craziness,’ but the person’s best attempt to soothe enormous fear in a world where they still feel unsafe.
It’s really about finding the meaning of the client’s choice, whether that choice is food restriction, binging, purging, overeating, or other self-harming. It’s felt to the personal like a survival skill, and the person is doing the best they can.
Seeing the reason why a person is struggling with harmful behavior is SO important, because this is what makes possible the compassion necessary for healing.
“In the United States, 20 million women and 10 million men suffer from a clinically significant eating disorder at some time in their life”, reports the National Eating Disorders Association. We may notice someone changing to an unhealthy weight, but few of us know what to say or do.
The first step is to realize that every behavior has meaning. And if we can bring compassion to it, rather than judgment, we are more likely to help others find hope and healing, personal connection.
The Concept of ‘Health at Every Size’
I believe you can be healthy at any size. Nobody has to be a size 2. You can accept the body you have today and begin to walk the path of better self-care, beginning where you are.
A positive way that caring friends and family can help is to stop talking about food. Start asking gently to know what is going on for that person. Bring an attitude of understanding, support, and compassion for what you find.
The path to healthier coping skills is grounded in healthier relationships. People struggling with eating disorders need a supportive network of therapy, social support, friends, family, and self-care for recovery.
Healthy relationships enable us to develop healthy ways to manage emotions within a window of tolerance. For trauma survivors, these relationships are much harder to come by.
We all need compassion – especially people with eating disorders and other self-harming behaviors – to help us find healthier ways to calm down and feel all right.
More Resources
Related Articles by Robyn E. Brickel, MA, LMFT
- Do You Use Drugs and Alcohol to Manage Your Emotions?
- Healthy Relationships Matter More than We Think
- How to Talk With Your Adolescent About Their Drug or Alcohol Use
- Loving a Trauma Survivor: Understanding Childhood Trauma’s Impact On Relationships
- Trauma-Informed Care: Understanding the Many Challenges of Toxic Stress
- What Is Good Self-Care, and Why You Deserve It








Leave a Reply